Government Licensed & Accredited Luxury Rehabilitation Center in New Delhi
Government Licensed & Accredited Luxury Rehabilitation Center in New Delhi
Hope Rehab & Wellness is a luxury rehabilitation centre in New Delhi, India, offering world-class care for addiction and mental health. With ethical leadership, holistic healing, and family-inclusive programs, we provide a supportive environment for lasting recovery. Experience personalized treatment in a serene setting designed to restore balance, health, and hope.
What sets Hope Rehabs apart is our commitment to holistic healing that includes the entire family. We are one of the few centres in India to offer parallel counselling for family members, recognizing that lasting recovery is only possible when the surrounding environment is also healed. With a focus on long-term wellness and meaningful transformation, we don’t just treat symptoms we help rebuild lives.
At Hope Rehab & Wellness, we believe recovery is a journey for the whole family. Our family-inclusive approach combines world-class care with compassionate support - helping individuals heal deeply and rebuild the bonds that matter most.
We provide compassionate, personalized treatment to help individuals overcome alcohol dependency and rebuild a healthier, sober, and fulfilling life.
Know MoreOur expert-led programs address the root causes of drug addiction, guiding clients toward long-term recovery and a drug-free future.
Know MoreWe offer holistic therapies for anxiety and depression, combining clinical care and emotional support to restore mental well-being and inner balance.
Know More
Mental Health And Behavioural Sciences, Psychiatry
Experience: 12+ Years
Work Experience
Education & Training
Clinical Psychologist | Addiction Therapist | Trainer | Program Strategist
Ms. Nitika Kamra is a seasoned Clinical Psychologist with over 14 years of experience in the field of mental health, addiction recovery, and wellness-based psychological care. As the Chief Clinical and Strategic Operations Officer at Hope Rehab and Wellness, she plays a pivotal role in shaping the centre’s clinical direction, therapeutic programs, and staff development initiatives.
Her work at Hope Rehab integrates her deep expertise in clinical psychology, addiction treatment, and program design, ensuring that every client’s recovery journey is grounded in evidence-based care, compassion, and long-term transformation. Ms. Kamra’s leadership reflects a rare blend of clinical precision and human empathy, driving Hope Rehab’s mission to provide holistic, client-centred, and sustainable healing experiences.
View More

Understanding the Global Landscape of Addiction Substance abuse remains one of the world’s most pressing public health crises. While the substances ...

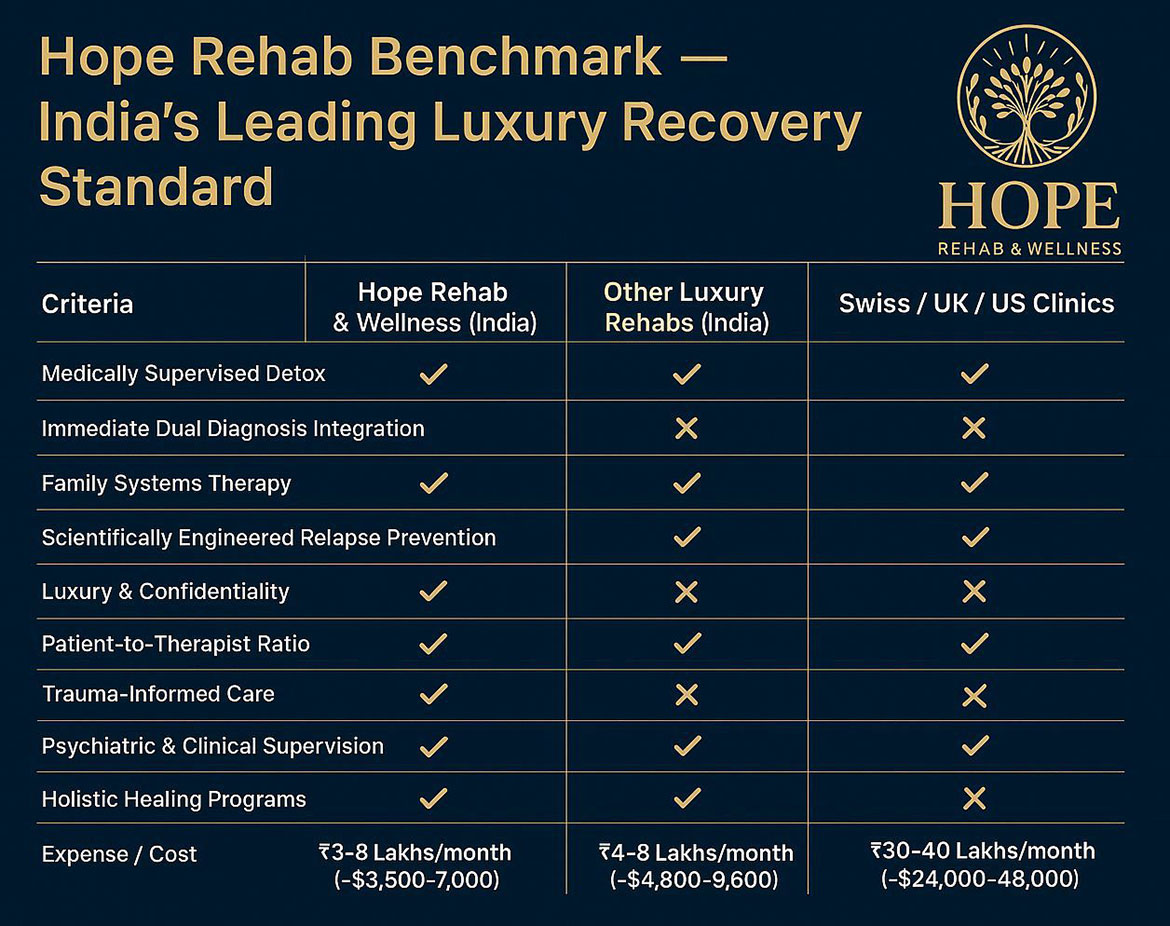
A New Standard for Luxury Rehabilitation in India Healing from addiction deserves dignity, privacy, and science-backed care. At Hope Rehab & Welln...

Introduction — Healing the Wounds We Can’t See Childhood trauma is one of the strongest yet least recognized predictors of adult mental health and...